
Common women’s health issues still painfully ignored
By HAZEL LOVE
Katey Da Silva had hundreds of medical visits, with dozens of doctors across two provinces. For years, her extreme pelvic pain and fatigue were dismissed as “normal for women” by health professionals.
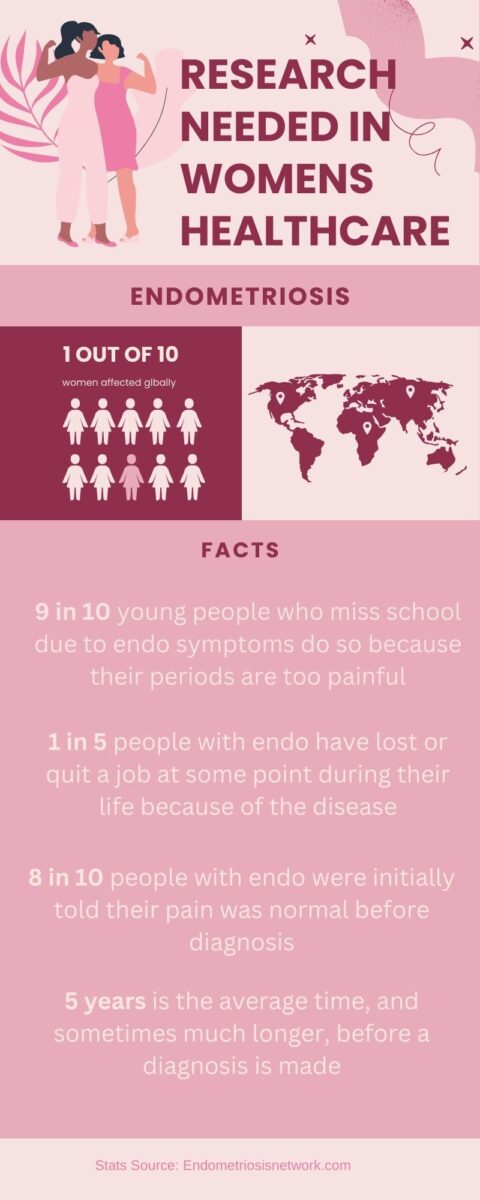
Da Silva, originally from Ontario, lived in British Columbia when she first experienced a myriad of health issues. At first, her symptoms were diagnosed as fibromyalgia and irritable bowel syndrome. However, these conditions were merely a symptom of a much larger problem rather than the root cause. Eventually, when she moved back to Ontario, she was diagnosed with endometriosis, a condition that affects one in ten women but often takes nearly a decade to identify, as well as Lyme disease.
Her story is not unique. Despite making up more than half the population, Canadian women often face significant barriers to adequate medical care and diagnosis.
A healthcare system that was never designed for women
Cheryl Warsh, a medical historian and professor at the University of Victoria, said gender bias in healthcare has been embedded in medical history for over two millennia. Ancient Greek physician Galen believed most female health issues stemmed from the uterus, coining the term hysterum, which later became hysteria.
The impact of systemic bias is felt acutely by women across Canada, many of whom spend years seeking answers for debilitating health conditions, only to be dismissed, misdiagnosed, or given inadequate treatment.
When Da Silva experienced an ovarian cyst rupture, she was met with condescension.
“One doctor brushed off my pain, saying, ‘So many women come in here with pelvic pain.’ Another compared my agony to a cyst in his ear. I was in excruciating pain, and he was equating it to that,” she said.
Historically, medical research has been centred around male bodies, leaving gaps in knowledge that persist today. The result is a healthcare system that frequently fails to recognize, diagnose, and treat conditions that disproportionately affect women.
“This idea, that women’s symptoms are ultimately linked to their reproductive system, has shaped medicine for 2,000 years,” Warsh said.
Even as medical understanding has evolved, biases persist. Warsh said that it was only 30 years ago that the medical community began recognizing that women present symptoms differently than men. However, medical equality still has a long way to go. Training, research, and treatment remain predominantly based on male bodies, she said.
Double discrimination in medicine
Women in Canadian healthcare face a dual burden, first as professionals and then as patients. Female surgeons earn less than their male counterparts, but an even more troubling statistic is that surgeries performed on female patients receive, on average, 28 percent lower reimbursement than those performed on men.
A 2023 study in the Canadian Journal of Surgery found that this issue is most pronounced in Saskatchewan, where the fee discrepancy reaches 67.3 per cent, in British Columbia, where it is 61.2 per cent, and in the Yukon, where it is 41.8 per cent.
The financial disparity raises fundamental questions about how medicine values bodies differently. Beyond the philosophical concerns, there are real-world consequences. Lower reimbursements for female patients may contribute to disparities in access to care, longer wait times, and resource allocation decisions.
“How do they justify that?” Warsh said.
No baby, no treatment
Surgical intervention for endometriosis is often prioritized for individuals experiencing infertility. This focus on reproductive potential frequently leaves women suffering without treatment if they are not actively trying to conceive.
Da Silva said she felt she had no choice but to lie about wanting children in order to receive surgery for her endometriosis.
“I was told by friends that the only way they got the surgery was because they were trying to have a baby,” she said. “So I told my gynecologist that my boyfriend and I were getting serious and wanted to start trying soon. After that, I was finally put on the waitlist.”
This experience highlights a troubling pattern in women’s healthcare, where pain management and quality of life are deprioritized in favour of fertility outcomes.
The psychological toll of medical dismissal
Da Silva’s experience with medical gaslighting was no different when it came to her Lyme Disease. She began experiencing near-fainting spells, later diagnosed as Lyme carditis, a condition that weakens the blood vessels to the heart. Her doctor dismissed the symptoms as panic attacks.
“I was scared…but I didn’t feel anxious at all,” she said.
Eventually, after repeated dismissal, she started to believe that maybe it was anxiety. She agreed to try medication and was prescribed Effexor, an antidepressant often used to treat anxiety and chronic pain.
“It wasn’t helping my pain. So they kept increasing it and increasing it until I was overmedicated,” she said.
She was also prescribed sleeping pills but still wasn’t sleeping. Then, she started experiencing withdrawal symptoms and hypomania.
“I looked up the risks, and given my family history of mental health conditions, I was shocked my doctor even prescribed it to me,” she said.
She ultimately decided to stop taking the medication but withdrew too quickly, experiencing suicidal thoughts.
“I made it through, but it was awful,” she said, describing this as an extremely dark period of her life.
Punishment for self-advocacy
Women who seek second opinions or advocate for themselves are often labelled as difficult patients.
“The more sick I got, the less doctors wanted to help me,” Da Silva said. “Eventually, I was flagged in the system. If you go too often, they stop taking you seriously.”
Da Silva began travelling to hospitals in different regions so that she could see new doctors who hadn’t already dismissed her as a hypochondriac or pain medication addict.
Medical misogyny and the cost of ignorance
Jess Finnegan, a B.C. resident, experienced a range of symptoms for years, from irregular periods to persistent migraines. Her doctor repeatedly dismissed her concerns, advising her to stay on birth control.
“There’s too many people and too much waste in this world. If you aren’t ready to have a child, stay on the pill,” her doctor said.
Years later, she switched to a naturopath and was diagnosed with polycystic ovary syndrome, which the contraceptive pill can mask.
“Had I been taken seriously years ago and not had my hormones dismissed as “normal” and [doctors] put a contraception bandaid on it, I would have a much healthier body at this point of my life and not be navigating all of this in my mid-30s,” she said.
